
|
Dr. Kimberly Huynh D.C. |
|
|
June 26, 2025 · 8 min |
Whether it’s running, prolonged sitting, or simply walking up the stairs, knee pain is one of the most common
complaints we hear from patients. Knee pain affects people of all ages and is commonly caused by injury,
arthritis, or muscle imbalances. Symptoms can include stiffness, chronic discomfort, or even debilitating pain
that interferes with daily activities.
Knee pain may present in the anterior (front), lateral (outside), medial (inside), and/or posterior (back)
aspects of the joint. The location of pain, combined with the patient's history, mechanism of injury, and
physical examination findings, helps the chiropractor identify the underlying cause and create a personalized
care plan.
Below are seven of the most common causes of knee pain we treat – though many other knee conditions are also
assessed and managed in practice.

Seen in athletes and physically active individuals, patellofemoral pain syndrome (PFPS) is one of the most
common causes of anterior knee pain. A sudden increase in intensity or duration of physical activity can
overload the knee and lead to PFPS. Other causes include poor tracking of the kneecap, often due to hip or
foot misalignment.
Signs and symptoms of PFPS may include:
- Dull ache in front of the knee
- Sharp or stabbing pain with certain activities, especially with squatting
- Worsens with prolonged sitting or descending stairs
Chiropractic care includes assessing lower limb biomechanics, correcting misalignments, prescribing specific
exercises to strengthen muscles that aid in stabilizing the knee, such as the VMO, kinesiotaping, and
lifestyle changes, such as activity modifications, incorporating the RICE protocol, and recommendations for
orthotics when indicated.
Osteoarthritis (OA) is a degenerative joint disease known as wear and tear that occurs over time. OA is more
common with increasing age, gender (female), elevated body weight, and having a family history of OA, but can
be worsened by misalignment or prior injury.
Signs and symptoms of OA may include:
- Pain with weight-bearing
- Morning stiffness
- Reduced mobility
- Cracking or grinding sensation (crepitus) felt or heard during movement
- Temperature sensitivity (i.e. cold, damp weather)
Chiropractic care for knee pain often includes improving joint mobility, addressing compensatory issues in the
hips, spine, or ankles, and providing soft tissue therapy. Treatment plans may also incorporate low-impact
therapeutic exercises and evidence-informed lifestyle modifications, such as adopting an anti-inflammatory
diet and adjusting movement patterns to minimize joint stress.
A meniscus tear is a common knee injury involving damage to the C-shaped cartilage (meniscus) that cushions
the knee joint. Meniscus injuries can result from a traumatic event such as a sudden twisting injury,
hyperextension trauma, or excessive rotational load, or from chronic degeneration due to gradual wear and
tear. Meniscal injuries typically involve the medial or lateral joint line and may occur in conjunction with
MCL or ACL sprains.
Signs and symptoms of meniscus injuries may include:
- Deep knee pain
- Stiffness
- Joint line tenderness
- Antalgic gait
- Local swelling & redness
- Catching or locking of the knee
- Buckling of the knee
- Limited range of motion with difficulty bending or straightening the knee

If a meniscal tear is suspected, the chiropractor may perform special tests to help diagnose and may refer out for an MRI to confirm. Chiropractic care may include conservative measures such as gentle joint mobilizations, soft tissue therapy, and low-impact rehab therapy. If severe, surgery may be recommended.
IT band syndrome is the most common lateral knee pain. It occurs when the iliotibial band, a dense fibrous
band running on the outer thigh, becomes tight or inflamed and rubs against the lateral femoral condyle (outer
knee bone), especially during repetitive motion. Aggravating activities may include overtraining, running,
biking, or stairs, especially when on a decline.
Signs and symptoms of IT band syndrome may include:
- Diffuse lateral knee pain
- Tenderness
- Swelling
- Stiffness
- Popping
Chiropractic care may include correcting spinal and pelvic alignment, assessing foot biomechanics, providing
soft tissue therapies such as instrument-assisted techniques, and prescribing targeted stretches, foam
rolling, and strengthening exercises for the glutes and hip muscles. Custom orthotics may also be recommended
to support proper lower limb mechanics.
The knee is supported by four major ligaments that help stabilize the joint during movement. Ligamentous injury, or sprain, occurs when these structures are overstretched or torn. Sprains are classified by severity: Grade I (mild fiber disruption), Grade II (partial tear), and Grade III (complete rupture).
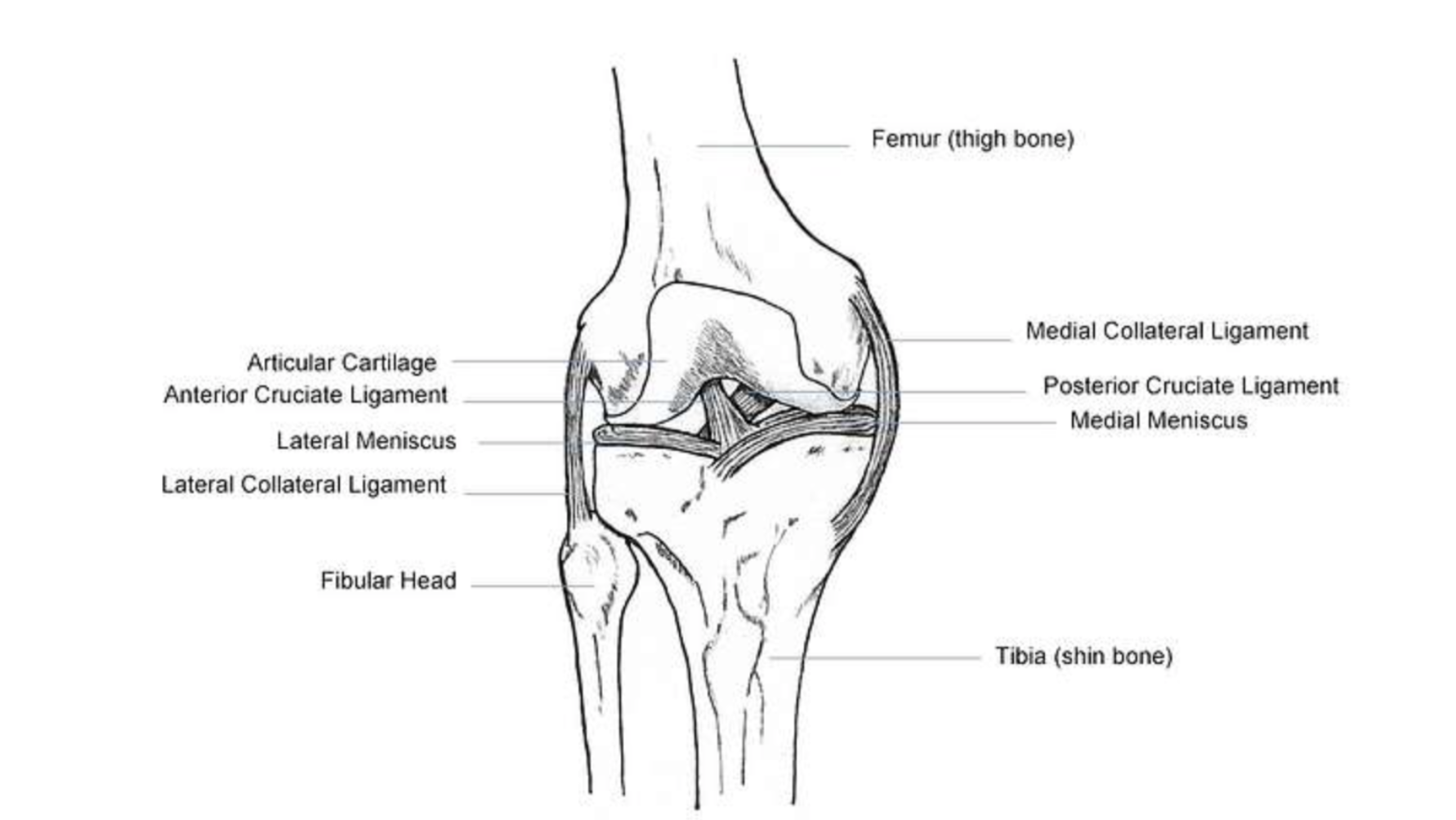
Image: Anatomy of the knee ligaments – via Picryl (Public Domain)
The medial collateral ligament (MCL) is the most common knee ligament injury. It provides stability to the
inner (medial) side of the knee. Often caused by valgus force (blow to the outside of the knee), or twisting
injury with the foot planted.
The anterior cruciate ligament (ACL) prevents the tibia from sliding forward under the femur. ACL tears are
also common, especially in athletes, typically non-contact due to sudden stops, pivots, or jumps.
Lateral collateral ligaments (LCL) are less common sprains and are usually caused by a varus force (blow to
the inside of the knee). The LCL provides stability to the outer (lateral) knee
Posterior cruciate ligament (PCL) is the least common of all four sprains, and typically results from direct
impact to a bent knee (i.e. dashboard injury). The PCL prevents the tibia from sliding backward under the
femur.

Chiropractic care can play a supportive role in both post-surgical rehabilitation and non-surgical management of knee sprain injuries. Interventions may include gentle joint mobilizations and spinal, hip, or foot adjustments to address compensatory biomechanical dysfunction. Additional treatment modalities may involve soft tissue therapy, kinesiotaping, and targeted rehabilitation exercises aimed at strengthening key muscle groups such as the quadriceps, hamstrings, and gluteal muscles.
Not all knee pain originates from the knee itself. Often, nearby surrounding structures such as the lower back
and hip can radiate pain down towards the knee and can mimic knee pain. Conditions like sciatica, lumbar disc
irritation, facet joint dysfunction, or hip joint issues (such as early arthritis or impingement) can cause
discomfort that radiates down the leg and is misinterpreted as knee pain.
Knee pain may occur during walking, prolonged sitting, or transitioning from sitting to standing, even without
a clear history of injury, and is often described as dull, achy, or intermittent.
Chiropractic care includes assessing beyond the knee to assess the full kinetic chain. Care may include
chiropractic adjustments, soft tissue therapy, gait and postural correction, and targeted rehab for the core,
glutes, and stabilizing muscles.
Flat feet, collapsed arches, or overpronation (when the foot rolls inward excessively while walking or
running) can cause the knee to rotate inward, disrupting natural alignment and placing strain on the
ligaments, tendons, and cartilage of the knee joint. Poor foot mechanics change the way the body absorbs shock
and moves through each step. Over time, this can lead to knee issues like patellofemoral pain syndrome, IT
band syndrome, or even degenerative joint changes. This often goes unnoticed, as symptoms present in the knee
despite the root cause originating from the feet.
Chiropractic care includes assessing the entire lower kinetic chain, from the feet and ankles all the way to
the hips and pelvis, to identify and correct biomechanical dysfunction. Treatment may include foot and ankle
adjustments, custom orthotics, footwear recommendations, gait retraining, correcting posture, increasing
awareness of weight distribution, and strength and stability rehab for the foot muscles, ankle, glutes, and
hips.
- If your pain lingers >1-2 weeks
- If you notice swelling, popping, or instability
- If rest, ice, and self-care aren’t helping
Chiropractic care offers a natural, non-invasive approach to managing knee pain. In addition to chiropractic
adjustments, targeted home exercises and lifestyle education can help strengthen muscles, improve mobility,
and reduce pain. Early intervention can prevent long-term issues or surgery.
Are you dealing with nagging knee pain? Book a consultation to determine the cause of your knee pain and
explore your treatment options. Give us a call at (604) 496-0626, email at info@paradisechiropractic.ca, or
book online.
Gaitonde DY, Ericksen A, Robbins RC. Patellofemoral Pain Syndrome. Am Fam Physician. 2019 Jan 15;99(2):88-94.
PMID: 30633480.
Vizniak, N. A. (2021). Hip knee ankle & foot pain (1st ed.). Professional Health Systems.