
 |
Author: Dr.Kimberly Huynh March 31, 2025 · 4 min |

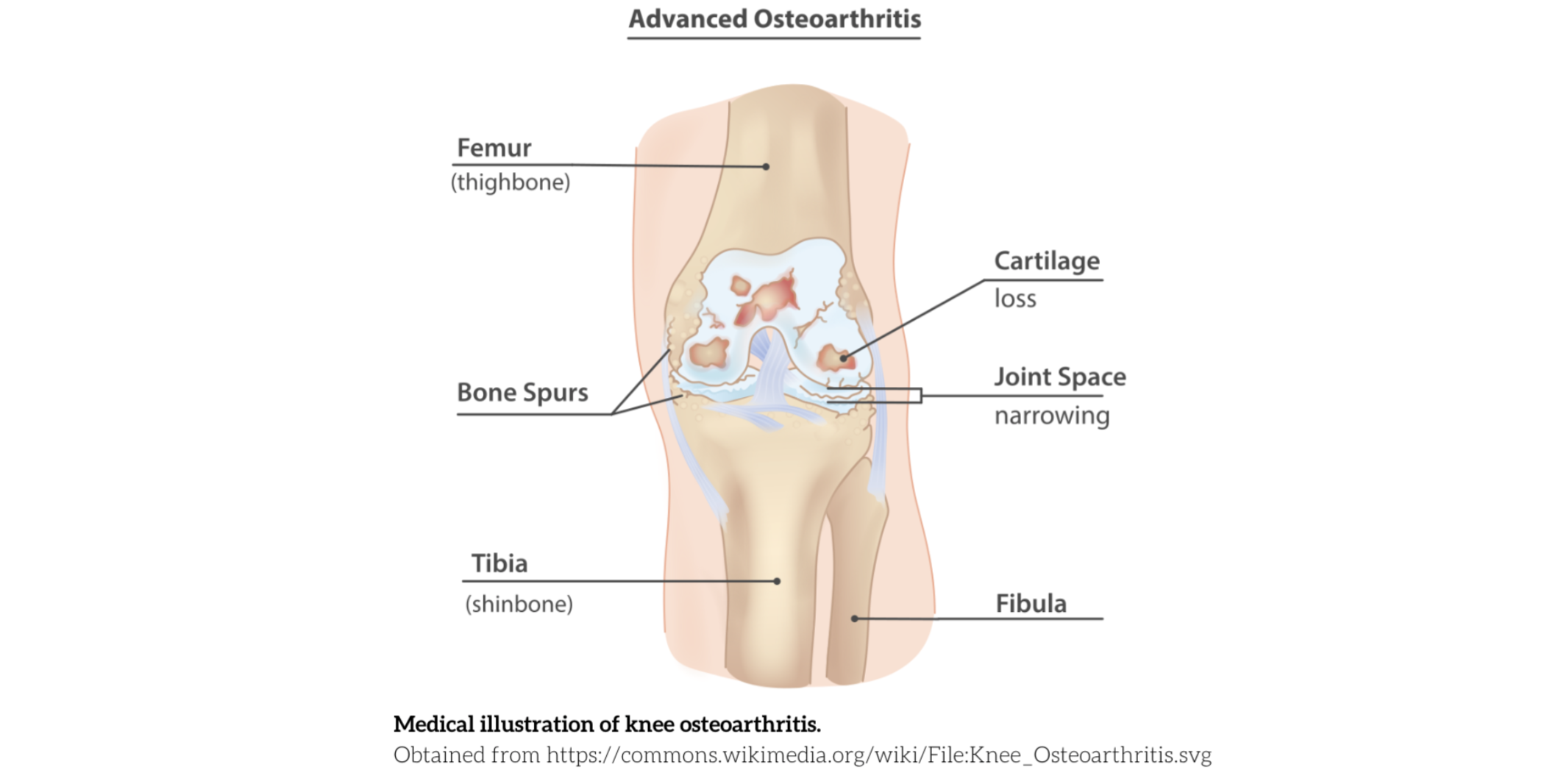
Osteoarthritis (OA) is the most common form of arthritis in adults, characterized by joint inflammation and structural changes that cause chronic pain, mobility loss, and functional disability. According to Young et al., hip and knee OA rank 12th in global disability. It can coexist with and negatively impact other chronic conditions, further decreasing quality of life and functional ability. In Canada, nearly 4 million people have osteoarthritis, with over 122,000 knee and hip replacements performed each year.
Hip and knee osteoarthritis typically progresses with age and weight gain. Non-modifiable risk factors—those that cannot be changed—include being over 40 years of age, being female, and having a genetic predisposition. Modifiable risk factors, which can be addressed through lifestyle changes, include excess weight, physical inactivity, previous joint injuries, muscle weakness, and repetitive high-impact activities that place excessive stress on the joints.
The presentation of osteoarthritis varies among individuals but may include:
• Stiffness, especially in the morning
• Swelling and inflammation
• Reduced range of motion (i.e. difficult bending, straightening, or rotating hip or knee)
• Bony enlargement
• Crepitus (grinding or cracking sensation)
• Joint pain with movement and weight-bearing activities
• Weakness and instability
Various conservative management options exist for hip and knee osteoarthritis, allowing individuals to choose
a multimodal approach that best suits their needs. Evidence-based treatments can effectively reduce pain,
enhance function, and improve overall quality of life.
Understanding hip and knee OA, its progression, and the role of self-management is integral to maintaining joint health.
Implementing joint protection strategies and lifestyle modifications can help slow its advancement and
alleviate symptoms. This may include setting realistic goals, allowing individuals to take control of their
condition and track progress effectively. Additionally, identifying and modifying activities that exacerbate
pain can reduce joint stress, enhance comfort, and improve overall function.
Examples include:
• Using an anti-fatigue mat in the kitchen.
• Having appropriate footwear.
• Limiting high-impact activities and opting for lower-impact activities.
• Weight loss if necessary.
• Staying hydrated.
• Getting enough sleep.
By combining these strategies, individuals with OA can better manage their symptoms and continue engaging in
meaningful activities with greater ease.
Exercise is one of the cornerstones of hip and knee osteoarthritis management. Depending on the stage of OA and each individual’s physical ability, exercise therapy may include: Strengthening exercises targeting the muscles surrounding the affected joint (e.g., quadriceps, hamstrings, gluteals) to improve joint stability and reduce pain. Range of motion exercises to maintain joint flexibility and prevent stiffness. Low-impact aerobic exercises, such as walking, swimming, or cycling, to improve cardiovascular health, reduce pain, and enhance overall function. Neuromuscular exercises that improve balance and proprioception can enhance joint stability and reduce the risk of falls.

The GLA:D (Good Life with Arthritis in Denmark) protocol is an evidence-based structured exercise and education program specifically for hip and knee OA. For more information, click HERE
Weight loss may be considered for individuals with excess weight, as even a modest reduction can significantly decrease joint stress and pain. Alongside dietary changes, regular physical activity can help support healthy weight management.
Chiropractic therapy, including adjustments, can improve joint mobility, reduce stiffness, and alleviate pain. This can be especially useful for hip and knee osteoarthritis, where joint restrictions are common. In addition, soft tissue therapy can address muscle tension and trigger points surrounding the affected joint and can improve pain and function. Chiropractic care often includes personalized exercise programs and education on posture and ergonomics to support long-term joint health. Studies have shown that chiropractic manipulation and mobilization, in conjunction with exercise, can provide clinically significant improvements in pain and function for hip and knee osteoarthritis. Other non-surgical conservative therapies that may be beneficial include physiotherapy, massage therapy, and acupuncture.
In conjunction with other treatments, these physical modalities may aid in OA symptoms such as:
• Heat and cold therapy to provide temporary pain relief and reduce inflammation.
• Transcutaneous Electrical Nerve Stimulation (TENS) to modulate pain signals and provide pain
relief.
• Ultrasound therapy to promote tissue healing and reduce pain.
Using assistive devices such as canes or walkers can reduce weight-bearing stress and improve stability. Other assistive devices include orthotics, which can provide proper foot alignment to support and improve joint alignment. Consult with your chiropractor or other health professionals to determine if this is appropriate for you.

Pharmacological management may include over-the-counter pain relievers such as NSAIDs (nonsteroidal anti-inflammatory drugs) or acetaminophen, which can provide temporary symptom relief. Topical pain relievers, like creams or gels containing menthol or capsaicin, can also help by numbing the affected area. In some cases, corticosteroid or hyaluronic acid injections may be used to reduce inflammation and improve joint lubrication, though they are often considered adjunctive treatments. Always consult a medical doctor or healthcare professional for personalized guidance on medication use.
A multimodal approach combining education, exercise, manual therapy, and lifestyle modifications is effective
for conservative management of hip and knee OA. By implementing these evidence-based conservative strategies,
individuals with hip and knee osteoarthritis can effectively manage their symptoms, improve function, and
enhance their overall quality of life.
Seek care from our experienced multidisciplinary team, who can provide comprehensive and individualized
treatment. Give us a call at (604) 496-0626, email at info@paradisechiropractic.ca, or book online.
(1) Dong Y, Yan Y, Zhou J, Zhou Q, Wei H. Evidence on risk factors for knee osteoarthritis in middle-older
aged: a systematic review and meta analysis. J Orthop Surg Res. 2023 Aug 29;18(1):634. doi:
10.1186/s13018-023-04089-6. PMID: 37641050; PMCID: PMC10464102.
(2) Public Health Agency of Canada. (n.d.). Osteoarthritis. Government of Canada. Retrieved March 20, 2025,
from https://www.canada.ca/en/public-health/services/publications/diseases-conditions/osteoarthritis.html
(3)Young JJ, Perruccio AV, Veillette CJH, McGlasson RA, Zywiel MG. The GLA:D® Canada program for knee and hip
osteoarthritis: A comprehensive profile of program participants from 2017 to 2022. PLoS One. 2023 Aug
3;18(8):e0289645. doi: 10.1371/journal.pone.0289645. PMID: 37535587; PMCID: PMC10399832.
(4) Young, J. J., Važić, O., & Cregg, A. C. (2021). Chiropractic care for older adults (Issue 65). Canadian
Chiropractic Association. Retrieved from
https://chiropractic.ca/wp-content/uploads/2021/05/120503-1_Chiro_65_1b_Young.pdf